What is a nuclear exercise stress test?
A nuclear exercise stress test is a diagnostic test used to evaluate blood flow to the heart. During the test, a small amount of radioactive tracer is injected into a vein. A special camera, called a gamma camera, detects the radiation released by the tracer to produce computer images of the heart.
Combined with exercise, the test can help determine if there is adequate blood flow to the heart during activity versus at rest.
Can I eat or drink on the day of the test?
Yes. However, DO NOT eat or drink anything but water for 4 hours before the test. If you must take medications, drink only drink water to help you swallow your pills.
Avoid all products containing caffeine for 24 hours before the test. In general, caffeine is found in coffee, tea, colas, Mountain Dew®,chocolate and decaffeinated products. Decaffeinated products contain trace amounts of caffeine.
Should I take my medications the day of the test?
Please bring all of your medications, including over-the-counter medications and supplements that you routinely take, to the test appointment.
Please follow these guidelines about taking your medications the day of the test.
- Medications with caffeine: DO NOT take any over-the-counter medication that contains caffeine (such as Excedrin®, Anacin®, diet pills and No Doz®) for 24 hours before the test. Ask your physician, pharmacist or nurse if you have questions about other medications that may contain caffeine.
- If you have asthma: Please bring your asthma inhaler medication to the test.
- If you have diabetes: If you take medications to control your blood sugar, do not take your medication until after the test is complete. Bring your diabetes medications with you so you can take it when the test is complete. Do not take your diabetes medication and skip a meal before the test. Plan to eat and take your blood sugar medication following your test.
What should I wear for the test?
- Please wear comfortable 2 piece clothing and shoes suitable for walking during the test. Ladies, it's preferable you not wear dresses or skirts.
- Please DO NOT wear sandals.
- Do not wear any clothing that has metal on the shirt. This includes metal snaps on shirts.
Please DO NOT bring children with you to the testing. We are using radiation for your testing and there will be several other patients like yourself here. Therefore, you will not want children or anyone pregnant exposed unnecessarily to the radiation.
What to expect during the test
The testing area is supervised by a physician.
A nuclear medicine technologist will place an IV into a vein in your arm or hand and inject a small amount of radioactive tracer. The tracer is not a dye or contrast. After the tracer is injected, you will wait approximately 1 hour before the first set of “resting” images are taken.
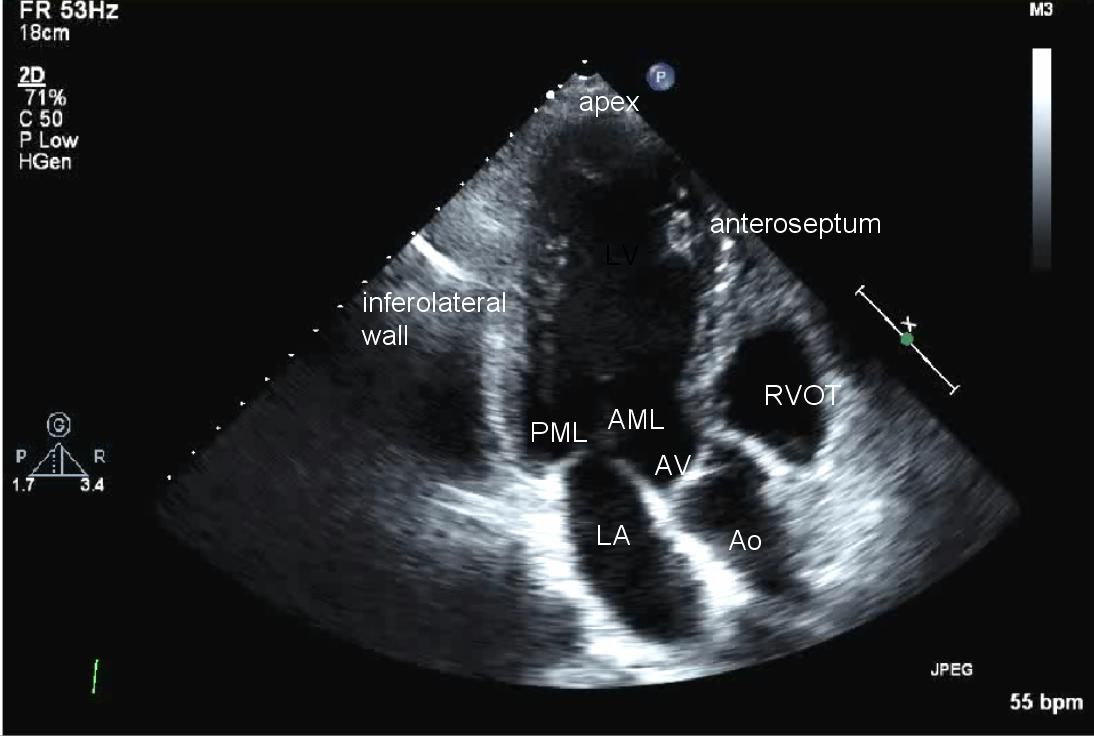
Then you will be asked to lie very still under the gamma camera with both arms above your head for about 7 minutes. The camera will record images that show blood flow through your heart at rest.
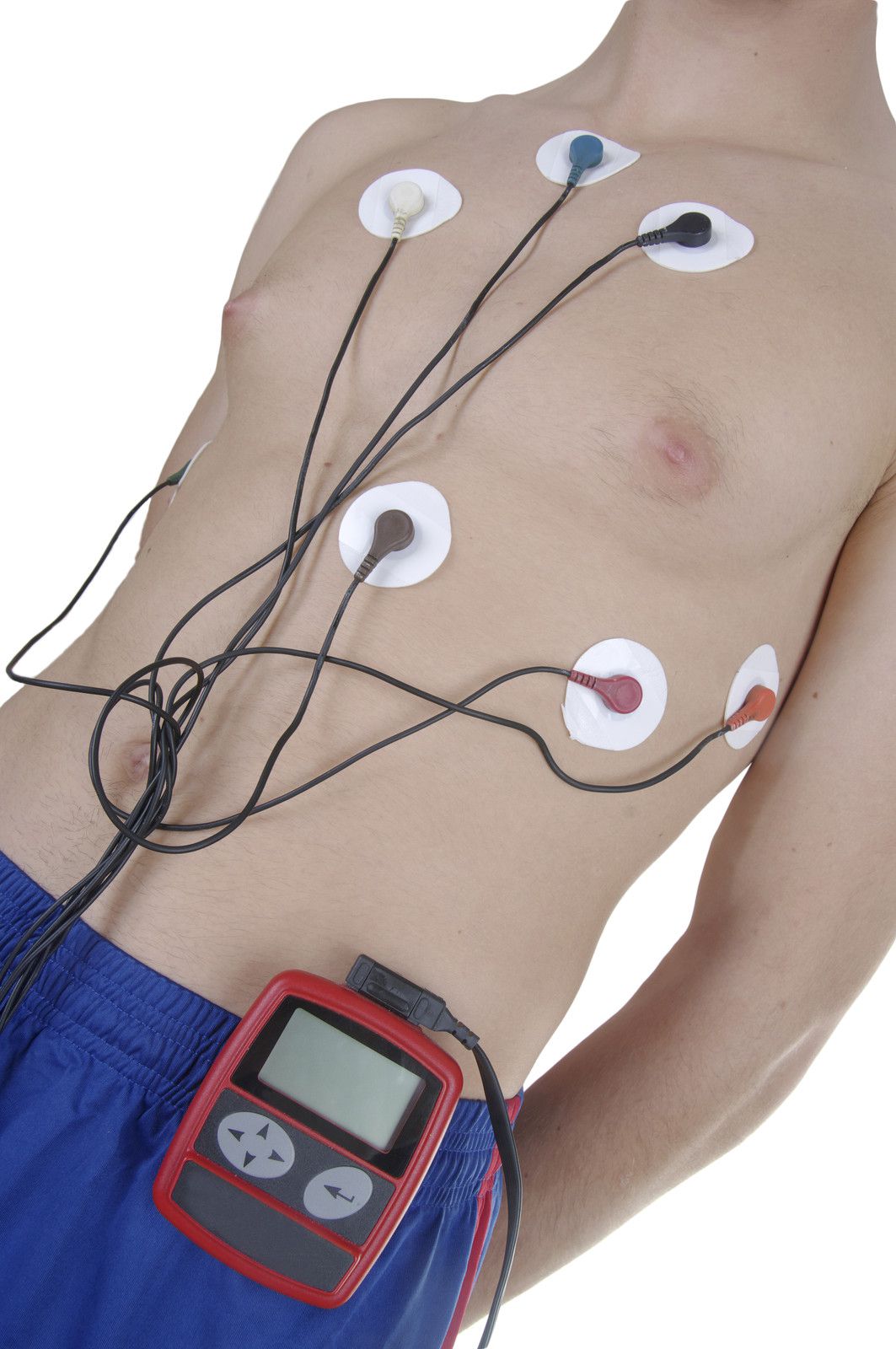
Next, a technician will place electrodes on your chest to monitor your EKG while you exercise.
You will walk on a treadmill. At regular intervals, the difficulty of the exercise will increase until you achieve the target heart rate. Then, a second dose of radioactive tracer will be injected into the IV. Your heart rate, EKG and blood pressure will be monitored throughout the test. If you are unable to achieve your target heart rate or walk on a treadmill, a medication will be given to simulate exercise.
After you have exercised, you will be offered a snack of coffee or juice and crackers. You may also bring a snack from home, if you prefer. Caffeine is permitted AFTER you have exercised.
About 45 minutes after exercising, you will be asked to again lie very still under the camera with both arms over your head for about 5 minutes. The camera will record images that show blood flow through your heart during exercise. These images will be compared to the first set.
How long will the test last?
The appointment will take about 3 to 4 hours. The actual exercise part of the test usually lasts about 5-12 minutes.
What if I need to reschedule my test?
If you are unable to keep your appointment, please notify our office at least 24 hours in advance. Failure to do so may result in forfeiture of your deposit.
How do I get the results of my test?
After the cardiologist reviews your test, the results will go into your electronic medical record. Your referring physician will have access to the results and will contact you to discuss them.












FOLLOW US